Introduction: The Heel’s Hidden Agony
Retrocalcaneal bursitis, often overshadowed by its more famous counterpart, Achilles tendonitis, is a condition that can bring even the most active individuals to a halt. The pain, swelling, and discomfort associated with this ailment can be debilitating, but with proper understanding and timely intervention, it can be managed effectively. This article delves deep into the intricacies of retrocalcaneal bursitis, offering insights into its causes, symptoms, and the latest treatments.
Why This Matters
In our fast-paced world, mobility is paramount. Whether you’re an athlete pushing your body to its limits, a professional clocking thousands of steps in a corporate setting, or simply someone enjoying a leisurely walk in the park, the health of your feet is crucial. Retrocalcaneal bursitis, if left unchecked, can significantly hamper this mobility. Moreover, understanding this condition is not just about addressing pain—it’s about preserving the quality of life.
A Journey of Discovery
As we navigate the depths of retrocalcaneal bursitis, we’ll uncover the anatomy of the heel, the subtle signs that might indicate the onset of this condition, and the myriad of treatment options available. From home remedies to advanced medical interventions, this article promises a comprehensive look at a condition that deserves more attention than it often receives.
Setting the Stage
Before we dive into the specifics, it’s essential to lay a foundation. The next section will demystify what retrocalcaneal bursitis is, differentiating it from other foot-related ailments and setting the stage for a deeper understanding of its causes and symptoms.
What is Retrocalcaneal Bursitis?
The Anatomy of the Heel
To truly grasp the nature of retrocalcaneal bursitis, one must first understand the intricate anatomy of the heel. The heel is more than just the back part of the foot; it’s a complex structure made up of bones, tendons, ligaments, and bursae.
- The Calcaneus: This is the heel bone, the largest bone in the foot, designed to bear the body’s weight during walking and running.
- Achilles Tendon: Connecting the calf muscles to the calcaneus, this tendon plays a pivotal role in foot movement, especially during activities like running, jumping, and climbing.
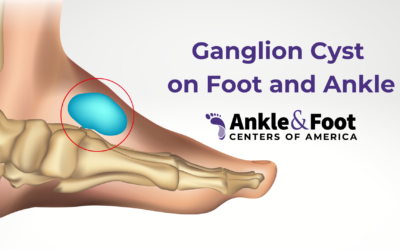
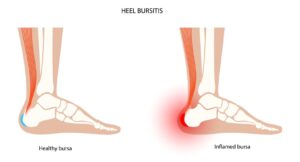
- Bursae: These are small, fluid-filled sacs located throughout the body, acting as cushions between bones and soft tissues like tendons and muscles. The heel has several bursae, but the one situated between the Achilles tendon and the calcaneus is called the retrocalcaneal bursa.
Defining Retrocalcaneal Bursitis
Retrocalcaneal bursitis occurs when the retrocalcaneal bursa becomes inflamed. This inflammation can result from various factors, leading to symptoms like pain, swelling, and redness at the back of the heel.
- Inflammation: At its core, bursitis is an inflammatory condition. When the bursa is subjected to repeated pressure or friction, it can become irritated, leading to inflammation.
- Symptom Onset: Unlike some conditions that manifest suddenly, retrocalcaneal bursitis often starts subtly. It might begin as a mild discomfort after a long run or a day in ill-fitting shoes, gradually intensifying if left unaddressed.
Differentiating from Other Foot Ailments
Given the foot’s complexity, several conditions can mimic the symptoms of retrocalcaneal bursitis:
- Achilles Tendonitis: This involves inflammation of the Achilles tendon itself, rather than the bursa. While both conditions can cause heel pain, the location and nature of the pain might vary.
- Plantar Fasciitis: Another common cause of heel pain, this condition affects the plantar fascia, a thick band of tissue connecting the heel bone to the toes.
- Haglund’s Deformity: Often associated with retrocalcaneal bursitis, this bony enlargement on the back of the heel can aggravate the bursa, leading to inflammation.
Understanding these distinctions is crucial for accurate diagnosis and effective treatment.
The Role of Biomechanics
Foot biomechanics, or the study of movement in the foot, plays a significant role in the onset of retrocalcaneal bursitis. Factors like gait, arch type, and even the kind of footwear one uses can influence the pressure distribution in the foot, potentially leading to conditions like bursitis.
Causes and Symptoms
Unraveling the Root Causes
Understanding the triggers and underlying causes of retrocalcaneal bursitis is pivotal for both prevention and treatment. While some factors are inherent, others are a result of external influences or lifestyle choices.
- Repetitive Strain: Activities that put consistent strain on the heel, such as long-distance running, frequent jumping, or even prolonged walking, can lead to irritation of the retrocalcaneal bursa.
- Improper Footwear: Shoes that don’t fit well or lack proper support can cause undue friction or pressure on the bursa. High heels or shoes with a rigid back can be particularly problematic.
- Foot Structure: Individuals with certain foot structures, like a high arch or flat feet, might be more prone to developing bursitis due to uneven weight distribution.
- Underlying Health Conditions: Conditions like rheumatoid arthritis or gout can predispose individuals to various forms of bursitis, including retrocalcaneal bursitis.
- Trauma: Direct injury to the heel, such as a fall or a hit, can lead to inflammation of the bursa.
Symptoms: More than Just Pain
 While pain is a primary indicator of retrocalcaneal bursitis, several other symptoms can provide clues to its presence:
While pain is a primary indicator of retrocalcaneal bursitis, several other symptoms can provide clues to its presence:
- Swelling: The area at the back of the heel might appear swollen, sometimes accompanied by warmth.
- Redness: The inflamed bursa can cause the skin over the heel to become red.
- Stiffness: The affected heel may feel stiff, especially in the morning or after prolonged periods of rest.
- Tenderness: The area might be sensitive to touch or pressure, making it uncomfortable to wear certain shoes.
- Audible Symptoms: In some cases, there might be a creaking sound when flexing the foot or ankle, known as crepitus.
The Role of Haglund’s Deformity
As previously mentioned, Haglund’s deformity, a bony enlargement on the back of the heel, can exacerbate retrocalcaneal bursitis. But how does this interplay work?
- Friction: The bony prominence can rub against the retrocalcaneal bursa, leading to irritation and inflammation.
- Pressure: The deformity can exert additional pressure on the bursa, especially in tight or rigid shoes.
- Compounded Symptoms: Those with Haglund’s deformity might experience intensified symptoms of bursitis due to the dual nature of their condition.
Biomechanics Revisited
Building on our earlier discussion of biomechanics, it’s essential to understand how specific gait patterns can contribute to bursitis:
- Overpronation: This occurs when the foot rolls inward excessively during walking or running, potentially leading to increased strain on the bursa.
- Oversupination: Conversely, some individuals’ feet roll outward too much, which can also lead to bursitis due to uneven pressure distribution.
- Stride Issues: A too-long or too-short stride can affect how the heel strikes the ground, potentially leading to bursitis over time.
The Importance of Accurate Diagnosis
Identifying retrocalcaneal bursitis accurately is paramount. A misdiagnosis can lead to ineffective treatments, prolonged pain, and potential complications. The diagnostic process involves a combination of clinical examinations, patient history, and imaging techniques.
Clinical Examination
A thorough physical examination by a healthcare professional, usually a podiatrist or orthopedic specialist, is the first step:
- Palpation: By feeling the affected area, the doctor can assess the degree of tenderness, swelling, and warmth, which can provide clues about the inflammation’s severity.
- Range of Motion Tests: These tests help determine if the bursitis has affected the foot’s mobility. The doctor may ask the patient to flex, extend, or rotate the foot to gauge any discomfort or limitations.
- Gait Analysis: Observing the patient’s walking pattern can offer insights into biomechanical issues that might be contributing to the bursitis.
Patient History
Understanding the patient’s history is crucial for a holistic diagnosis:
- Activity Levels: Knowing the patient’s exercise habits, especially activities that put strain on the heel, can help pinpoint potential causes.
- Previous Injuries: Past traumas or injuries to the foot can predispose an individual to bursitis.
- Shoe Preferences: The type of footwear regularly worn can be a significant factor, especially if they lack support or fit poorly.
- Medical History: Underlying conditions like arthritis or gout can be contributing factors.
Imaging Techniques
While the clinical examination and patient history provide valuable insights, imaging techniques can offer a more in-depth look:
- X-rays: While X-rays won’t show the inflamed bursa, they can reveal bone deformities, like Haglund’s deformity, or other bone-related issues that might be contributing to the inflammation.
- Ultrasound: This imaging technique can visualize soft tissues, making it useful for assessing the bursa’s state and the Achilles tendon.
- MRI (Magnetic Resonance Imaging): An MRI provides detailed images of both soft tissues and bones. It’s especially useful if the doctor suspects other conditions, like a tendon tear.
Differential Diagnosis
Given the foot’s complexity and the overlapping symptoms of various conditions, it’s essential to rule out other potential diagnoses:
- Achilles Tendonitis: As discussed earlier, this condition affects the tendon rather than the bursa. Imaging can help differentiate between the two.
- Plantar Fasciitis: Pain from this condition is typically focused on the bottom of the heel.
- Calcaneal Stress Fracture: Overuse can lead to small fractures in the heel bone, which can cause pain similar to bursitis.
The Path to Healing Without Surgery
 For many patients, the idea of surgery can be daunting. Fortunately, a majority of retrocalcaneal bursitis cases can be effectively managed with non-surgical treatments. These interventions aim to reduce inflammation, alleviate pain, and prevent recurrence.
For many patients, the idea of surgery can be daunting. Fortunately, a majority of retrocalcaneal bursitis cases can be effectively managed with non-surgical treatments. These interventions aim to reduce inflammation, alleviate pain, and prevent recurrence.
Home Remedies and Lifestyle Changes
Simple changes and remedies can make a significant difference:
- Rest: Giving the affected foot a break from strenuous activities can help reduce inflammation and speed up recovery.
- Ice Therapy: Applying ice to the inflamed area can help reduce swelling and provide pain relief. It’s recommended to ice the area for 15-20 minutes every few hours.
- Elevation: Elevating the foot can help reduce swelling, especially after prolonged activity.
- Footwear Modifications: Switching to shoes with a cushioned heel, soft back, and adequate arch support can reduce irritation.
Over-the-Counter Solutions
There are several readily available solutions that can aid in the treatment:
- Pain Relievers: Non-prescription pain relievers like ibuprofen or naproxen can help reduce pain and inflammation.
- Heel Pads: These can be placed inside shoes to provide additional cushioning, reducing pressure on the bursa.
- Compression: Wearing a compression bandage can help support the affected area and reduce swelling.
Physical Therapy and Exercises
Guided exercises can strengthen the foot’s muscles, improve flexibility, and reduce the risk of recurrence:
- Stretching: Gentle stretches targeting the Achilles tendon and calf muscles can alleviate tension and reduce strain on the bursa.
- Strengthening Exercises: Building strength in the foot and calf muscles can provide better support and reduce the risk of future flare-ups.
- Ultrasound Therapy: Some physical therapists use ultrasound waves to promote tissue healing and reduce inflammation.
Custom Orthotics and Support
For those with specific foot structures or gait patterns contributing to bursitis:
- Custom Insoles: These are designed to address individual biomechanical issues, redistributing pressure and providing support.
- Arch Supports: Especially beneficial for those with flat feet or high arches, these can help evenly distribute weight across the foot.
Corticosteroid Injections
For severe or persistent cases:
- Direct Relief: A corticosteroid, often combined with a local anesthetic, can be injected into the inflamed bursa to provide rapid relief from pain and inflammation.
- Caution: While effective, repeated corticosteroid injections can weaken the Achilles tendon, increasing the risk of rupture.
It’s essential to discuss the benefits and risks with a healthcare professional.
Alternative Therapies
Some patients find relief with alternative treatments:
- Acupuncture: This ancient technique involves inserting thin needles into specific points to alleviate pain.
- Massage Therapy: Targeted massage can help reduce muscle tension, improve circulation, and promote healing.
When Non-Surgical Interventions Aren’t Enough
While many patients find relief with non-surgical treatments, there are instances where these methods might not provide the desired results or where the condition is too severe. In such cases, advanced treatment options, including surgical interventions, come into play.
Surgical Interventions
For those with chronic retrocalcaneal bursitis or associated complications like Haglund’s deformity, surgery might be the best option:
- Bursa Removal (Bursectomy): This procedure involves removing the inflamed bursa. The body will eventually regenerate a new bursa over time.
- Haglund’s Deformity Correction: If the bony enlargement is contributing to the bursitis, it can be surgically removed to reduce pressure and friction on the new bursa.
- Achilles Tendon Detachment and Reattachment: In severe cases, the Achilles tendon might be temporarily detached to remove the bursa and, if necessary, address Haglund’s deformity. The tendon is then reattached.
Recovery and Rehabilitation
Post-surgery recovery is crucial to ensure the success of the procedure and prevent recurrence:
- Rest and Immobilization: The foot might be placed in a cast or boot to allow the surgical site to heal.
- Physical Therapy: Once the initial healing phase is over, guided exercises and stretches will be crucial to regain strength and flexibility.
- Return to Activity: It’s essential to gradually reintroduce activities to prevent overstraining the surgical site.
Prognosis
With proper post-operative care and adherence to rehabilitation:
- Success Rates: Most patients experience significant relief from pain and a return to their regular activities.
- Recurrence: While recurrence is possible, especially if underlying biomechanical issues aren’t addressed, the combination of surgery and post-operative care significantly reduces the chances.
Surgical interventions, while more invasive, offer a viable solution for those who don’t find relief with non-surgical treatments. The key is to work closely with healthcare professionals to determine the best course of action and ensure a comprehensive approach to recovery.
Alternative Therapies for Heel Bursitis Pain
Exploring Beyond Conventional Treatments
While mainstream medical treatments are effective for many, some individuals seek or supplement with alternative therapies. These methods, often rooted in traditional practices, can offer relief and a holistic approach to managing retrocalcaneal bursitis.
Acupuncture
A staple in traditional Chinese medicine, acupuncture has gained global recognition:
- Procedure: Thin, sterile needles are inserted into specific points on the body, known as meridians, to balance the body’s energy flow or “Qi.”
- Benefits: Many patients report reduced pain and inflammation after sessions. The exact mechanism remains a topic of research, but it’s believed to stimulate blood flow and release endorphins.
- Considerations: It’s essential to seek treatment from a licensed acupuncturist to ensure safety and effectiveness.
Herbal Remedies
Nature offers a plethora of herbs known for their anti-inflammatory properties:
- Turmeric: Curcumin, the active ingredient in turmeric, has potent anti-inflammatory effects. It can be consumed as a spice, tea, or supplement.
- Ginger: Similar to turmeric, ginger has anti-inflammatory properties and can be consumed in various forms.
- Topical Applications: Herbal ointments containing ingredients like arnica or capsaicin can be applied to the affected area for relief.
- Precautions: Before starting any herbal remedy, it’s crucial to consult with a healthcare professional to avoid potential interactions with other medications or conditions.
Hydrotherapy
The therapeutic use of water, in various temperatures and forms, can offer relief:
- Cold Compress: As discussed earlier, cold can reduce inflammation. Cold water soaks or ice packs can be beneficial.
- Warm Soaks: Warm water can relax muscles and improve blood circulation, aiding in the healing process.
- Contrast Baths: Alternating between cold and warm water soaks can combine the benefits of both, reducing inflammation and promoting healing.
Chiropractic Care
While chiropractic care primarily focuses on the spine, some practitioners offer treatments for foot ailments:
- Adjustments: Manipulations can help address biomechanical issues that might contribute to bursitis.
- Gait Analysis: Some chiropractors offer gait assessments to recommend corrective measures.
Homeopathy
This alternative medicine system uses highly diluted substances to stimulate the body’s healing:
- Common Remedies: Remedies like Rhus tox, Bryonia, and Arnica might be recommended for joint and tendon issues.
- Consultation: It’s essential to consult with a trained homeopath who can recommend the most suitable remedy based on individual symptoms.
Mind-Body Techniques
Managing pain isn’t just about physical treatments; mental well-being plays a role:
- Meditation and Relaxation: Techniques to calm the mind can help in pain management.
- Biofeedback: This method teaches individuals to control physiological functions to improve conditions like pain.
 Prevention and Long-Term Care
Prevention and Long-Term Care
The Proactive Approach to Heel Health
While treatments, both conventional and alternative, play a pivotal role in managing retrocalcaneal bursitis, prevention remains the most effective strategy. By understanding and implementing preventive measures, individuals can significantly reduce the risk of developing or re-experiencing this painful condition.
Footwear Choices
The shoes we wear can either be our best allies or our worst enemies when it comes to foot health:
- Proper Fit: Shoes should fit snugly without being too tight, especially around the heel area, to prevent unnecessary friction.
- Adequate Support: Footwear should provide good arch support, cushioning, and a flexible sole to distribute pressure evenly.
- Avoid High Heels: Regular use of high heels can strain the Achilles tendon, increasing the risk of bursitis.
- Alternate Shoes: Rotating between different pairs can prevent repeated pressure points and allow shoes to air out, reducing moisture and friction.
Biomechanical Considerations
Understanding and addressing individual biomechanical issues can be a game-changer:
- Orthotics: Custom-made insoles can correct abnormal foot mechanics, redistributing pressure and providing support.
- Gait Training: Physical therapists can offer guidance on walking techniques to reduce strain on the heel.
- Maintain a Healthy Weight: Excess weight can put additional pressure on the feet, increasing the risk of bursitis.
Exercise and Activity Modifications
Being active is essential, but it’s crucial to do so mindfully:
- Warm-Up and Stretch: Before engaging in physical activities, especially running or jumping, ensure you warm up and stretch the Achilles tendon and calf muscles.
- Gradual Increases: If you’re taking up a new sport or activity, increase intensity and duration gradually to give your body time to adjust.
- Listen to Your Body: At the first sign of heel discomfort, take a break. Pushing through pain can exacerbate the condition.
Regular Check-ups
Routine visits to a podiatrist or orthopedic specialist can help:
- Early Detection: Regular assessments can identify potential issues before they become problematic.
- Tailored Advice: Based on individual foot structure and lifestyle, professionals can offer personalized preventive strategies.
Holistic Health
Overall well-being can influence the health of your feet:
- Diet: Consuming anti-inflammatory foods like omega-3 rich fish, green leafy vegetables, and berries can help maintain low inflammation levels in the body.
- Hydration: Keeping well-hydrated ensures good tissue health, reducing the risk of injuries.
- Stress Management: Chronic stress can exacerbate inflammatory conditions. Techniques like meditation, yoga, and deep breathing can help manage stress.
Latest Research and Developments
Pushing the Boundaries of Heel Health Knowledge
The medical field is ever-evolving, with researchers continuously seeking better ways to understand, treat, and prevent conditions like retrocalcaneal bursitis. Staying updated with the latest research and developments ensures that patients and healthcare providers can make informed decisions based on the most recent evidence.
Advanced Imaging Techniques
While X-rays, ultrasounds, and MRIs have been the gold standard:
- 3D Imaging: Offers a more comprehensive view of the foot’s anatomy, allowing for precise diagnosis and treatment planning.
- Dynamic Ultrasound: Captures real-time movements, providing insights into how different activities affect the bursa and surrounding structures.
Novel Non-Invasive Treatments
Beyond the conventional non-surgical treatments:
- Shockwave Therapy: Uses acoustic waves to stimulate blood flow and promote tissue healing. Early studies suggest it may be beneficial for retrocalcaneal bursitis.
- Laser Therapy: Low-level lasers can reduce inflammation and accelerate tissue repair.
Biomechanical Innovations
Understanding foot mechanics has led to innovative solutions:
- Smart Insoles: Equipped with sensors, these insoles provide real-time feedback on pressure distribution, helping users make immediate corrections to their gait.
- 3D Printed Orthotics: Customized insoles based on 3D scans of an individual’s foot ensure a perfect fit and optimal support.
Regenerative Medicine
Harnessing the body’s healing capabilities:
- Platelet-Rich Plasma (PRP) Injections: Using a patient’s blood, PRP is concentrated and injected into the inflamed area, promoting healing.
- Stem Cell Therapy: While still in the experimental stages for bursitis, stem cells have the potential to regenerate damaged tissues.
Preventive Strategies
Research is also focusing on prevention:
- Footwear Materials: Exploring materials that reduce friction and provide better cushioning.
- Exercise Protocols: Developing routines specifically designed to strengthen the foot and reduce the risk of bursitis.
Patient-Centered Approaches
Recognizing that every patient is unique:
- Personalized Treatment Plans: Using genetic information and detailed biomechanical assessments to tailor treatments to individual needs.
- Digital Health Platforms: Apps and online platforms that allow patients to monitor their symptoms, track their progress, and stay connected with healthcare providers.
Staying abreast of the latest research and developments ensures that patients receive the best possible care. As science advances, the hope is to not only improve treatments for retrocalcaneal bursitis but also to enhance our understanding of its underlying causes, paving the way for more effective preventive strategies.
Conclusion
Reflecting on the Journey of Heel Health
From understanding the intricate anatomy of the heel to exploring the vast array of treatments, both conventional and alternative, our journey through retrocalcaneal bursitis has been comprehensive. As we conclude, it’s essential to reflect on the key takeaways and the path forward.
The Importance of Early Intervention
One of the most critical lessons is the value of early detection and intervention:
- Prompt Action: Addressing symptoms at their onset can prevent complications and reduce the need for more invasive treatments.
- Regular Check-ups: Even in the absence of symptoms, routine assessments can identify potential issues, ensuring proactive care.
Embracing a Holistic Approach
Heel health isn’t just about the foot:
- Whole-Body Health: Factors like diet, hydration, and stress management play a role in overall foot health.
- Mental Well-being: Recognizing the psychological impact of chronic pain and seeking support when needed is crucial.
Staying Informed
With the medical field continuously evolving:
- Latest Research: Patients and healthcare providers alike should stay updated with the most recent studies and developments.
- Open Dialogue: Regular communication between patients and professionals ensures that treatments are tailored to individual needs.
The Power of Prevention
While treatments are vital:
- Proactive Measures: Simple actions, like choosing the right footwear and incorporating foot-specific exercises, can make a world of difference.
- Awareness: Understanding the risk factors and being vigilant about potential symptoms ensures timely action.
Looking to the Future
With advancements in technology and medicine:
- Innovative Treatments: The future holds promise for even more effective and less invasive treatments for retrocalcaneal bursitis.
- Empowered Patients: Digital platforms and increased access to information empower patients to take charge of their health.
In the realm of foot health, knowledge is indeed power. By understanding retrocalcaneal bursitis in-depth, individuals can make informed decisions, ensuring not only the health of their heels but also their overall well-being. As we step forward, let’s do so with awareness, care, and a commitment to holistic health.